- Department of Neurosurgery, Sao Paulo Federal University (UNIFESP), Sao Paulo, Brazil
Correspondence Address:
Franz Jooji Onishi
Department of Neurosurgery, Sao Paulo Federal University (UNIFESP), Sao Paulo, Brazil
DOI:10.4103/sni.sni_114_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Franz Jooji Onishi, Samuel Salu, Sérgio Cavalheiro. Mobile cauda equina schwannomas: How to deal with this rare event and avoid surgical complications. 26-Jun-2018;9:125
How to cite this URL: Franz Jooji Onishi, Samuel Salu, Sérgio Cavalheiro. Mobile cauda equina schwannomas: How to deal with this rare event and avoid surgical complications. 26-Jun-2018;9:125. Available from: http://surgicalneurologyint.com/surgicalint-articles/mobile-cauda-equina-schwannomas-how-to-deal-with-this-rare-event-and-avoid-surgical-complications/
Abstract
Background:Mobile schwannomas of the cauda equina are rare. Preoperative planning should take into consideration the possibility of tumor migration, avoiding unnecessary additional laminectomy or second operation.
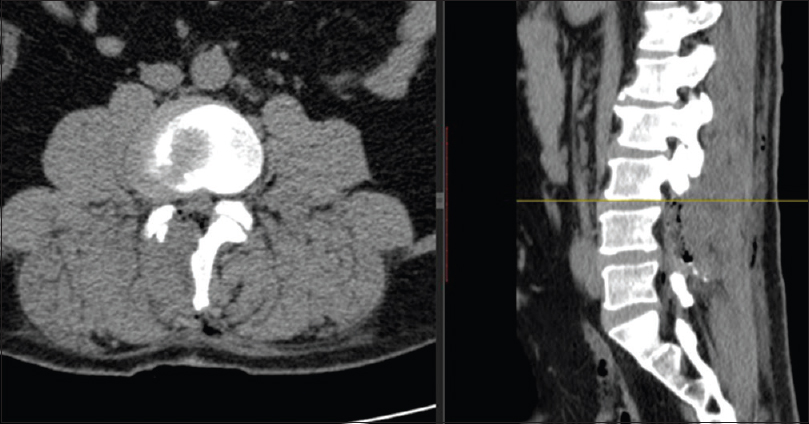
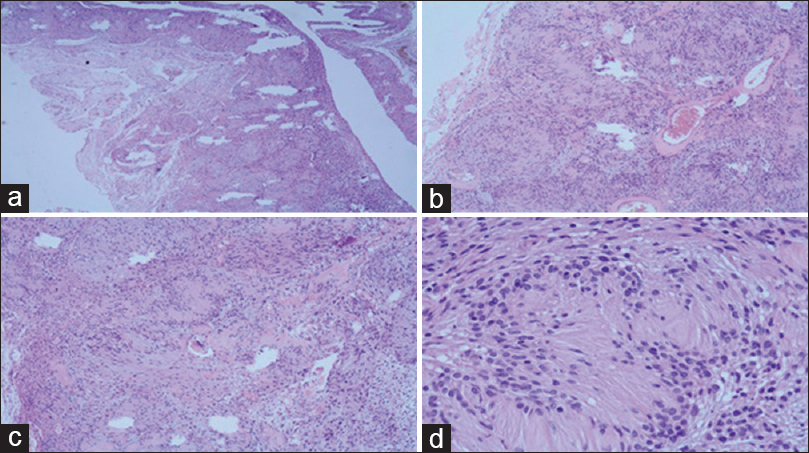
Case Description:A patient with a previously known lumbar schwannoma was being managed conservatively until symptoms exacerbated and led to a new MR. When this study revealed caudal migration of the schwannoma from L3 to the L4–L5 levels, a right hemilaminectomy was performed for tumor resection.
Conclusion:Great care must be taken in the surgical resection of schwannomas as they may migrate from their initial location.
Keywords: Causa equina, hemilaminectomy, nerve sheath neoplasms, perioperative care, radiculopathy
INTRODUCTION
Mobile tumors of the cauda equina, which migrate rostrally and/or caudally, are rare. Usually, they present with transient and paroxysmal pain. Despite recent magnetic resonance (MR) imaging done just several hours prior to surgery, schwannomas may migrate some levels away from the previously identified site. This may lead to unanticipated extensive laminectomies or reoperations. Various factors may contribute to such tumor migration including redundant nerve root, postural changes and/or, the thrust of the injected radiopaque material during myelography.
CASE HISTORY
A 49-year-old male presented with 4 years of recurrent back pain and increased clumsiness of the right leg. The neurological examination revealed gait impairment in both legs due to pain (no focal motor deficit), and a positive right-sided Lasègue maneuver.
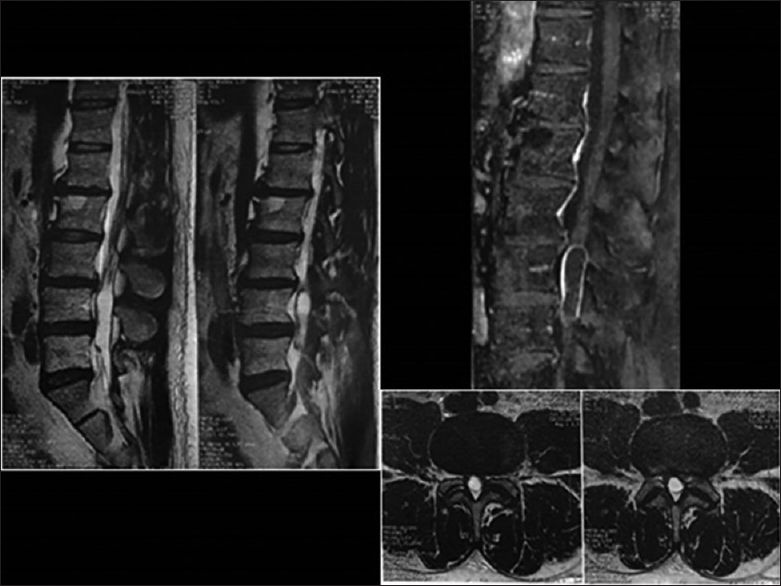
The initial (2015) unenhanced magnetic resonance imaging (MRI) showed a cystic lesion at the L3 level [
DISCUSSION
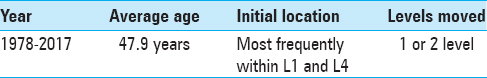
Mobile schwannomas of the lumbar spine are rare and have only been reported in 15 other cases [
There was only one report of possible tumor migration caused by trauma, with acute severe symptoms due to the incarceration of a mobile schwannoma after the patient's fall.[
Although rare, schwannomas involving the cauda equina are more likely to migrate versus those located in the cervical or thoracic spine.
Migration of lumbar schwannomas may lead to failed first operations that cannot successfully locate the tumor.[
The immediate preoperative localization made by MR can be confirmed with myelography[
Interestingly, migration of intradural lumbar schwannomas may occur both cephalad and caudad to the original tumor site.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Friedman JA, Wetjen NM, Atkinson JL. Utility of intraoperative ultrasound for tumors of the cauda equina. Spine (Phila Pa 1976). 2003. 28: 288-9
2. Kim SB, Kim HS, Jang JS, Lee SH. Mobility of intradural extramedullary schwannoma at spine: Report of three Cases with literature review. J Korean Neurosurg Soc. 2010. 47: 64-7
3. Marin-Sanabria EA, Sih IM, Tan KK, Tan JS. Mobile cauda equina schwannomas. Singapore Med J. 2007. 48: e53-6
4. Sasaki M, Aoki M, Yoshimine T. Mobile schwannoma of the cauda equina incarcerated following caudal migration after trauma--case report. Neurol Med Chir (Tokyo). 2011. 51: 710-2
5. Toscano DT, Felbaum DR, Ryan JE, Sayah A, Nair MN. Mobile schwannoma of the lumbar spine: A case report and review of the literature. Cureus. 2016. 8: e715-